Weight... Wait!
How much does it really matter what our bodies weigh? Does our worth and our values change in response to our mass? Must our happiness revolve around the scale? Is our health really measured by fat?

Why does anyone care about weight to height ratio? Is it because of health? Body image ideals? A desire to appease those around us to fit the mold of a professional, an athlete, or the perfect daughter? Because someone told you that you had to be a certain weight in order to hike that mountain, have a baby, or decrease your risk of disease?
Body weight not included, what do you care about? What makes you happy? What do you want from life? The answer to THESE questions are what health is. This is what should guide our actions, not our pounds.
Weight and Physical Health
The claims that extra weight contributes to chronic disease is debatable. The crux of the research reveals that it is the habits of health practice that result in prevention or risk of disease, not body weight alone, and these two are not mutually exclusive.
For example, evidence is strong that over consumption of added sugar can increase chronic disease risk, including cardiovascular disease and diabetes. You can consume a lot of added sugar, have it impact your blood pressure, cholesterol and blood sugar levels, and be “normal” weight, or “underweight”, or “obese”. You might never eat added sugar and be “normal” weight, or “underweight”, or “obese”. Your weight does not change the risk, the habit changes the risk.
Regardless of true cause and effect, the communication from the medical community and media that extra weight is harmful to our health is loud! Even worse is the message that we only have ourselves to blame if we have extra fat on our bodies. Little regard is given to the role of biology, the built environment, and fat shaming itself.
What may have started as a well-intentioned public health campaign to “stop obesity” to improve health has become a breading ground for discrimination towards those who are living in larger bodies. Body weight is an easy target as it cannot hide, such that it breeds weight bias.
You cannot determine a person’s health from how they look.
The newest recommendation of 5-10% weight loss in overweight and obese individuals in order to show significant decreases in disease risk, whether achieved or not, will not necessarily put those individual out of the overweight or obese categories. Therefore, regardless of weight change, or health risk change, the fear and reality of weight injustice is still there.
How would it feel if you successfully adapted your habits to ward off diabetes and are feeling health and excited! yet you still receive the same ridicule and assumption that you must be unhealthy because you still carry extra weight?
Why have we not learned from what has now been years of study that fat does not mean unhealthy? Fat also does not mean lazy, or uneducated, or ugly, or sloppy….

Weight and Mental Health
As mentioned, being fat is a visual, physical thing. It can not hide. What can hide, and does hide, is the mental, social and emotional implications of being fat. If we are talking about the impact of weight on health, these are the aspects of our wellbeing that should be addressed. America's diet culture and how society treats those living in a fat body is unhealthy.
The stress and anxiety of being labeled as overweight or obese is just as strong, if not stronger, of a risk factor on health as a person’s body weight. The mental turmoil placed on people in larger bodies can promote excessive cortisol release, leading to internal inflammation and related disease. It can also have the adverse effect of triggering appetite and poor food habits, adding to the fire of the weight versus health battle. Not to mention mental health illness such as depression and anxiety.
Example Case Study: Sharon is a 36 years old female with an enjoyable career and loving husband. She has never had any health issues and is not concerned about her weight. During a visit with a doctor for a hurt ankle Sharon is told she is overweight and needs to lose 20-30# “to be healthy”. For the first time, Sharon becomes negatively aware of her body size. Concerned, she goes on a highly restricted calorie diet. Sharon begins to lose weight quickly, but behind the scenes her stress hormones increase, her overall metabolism decreases, she becomes malnourished, fatigues, and disordered eating behaviors emerge. Due to these sudden biological changes Sharon stops losing weight before she reaches the doctor’s goal. She tries harder by going to the gym every day, but her weight won’t budge and actually starts to creep back up. Depressed at her failure she stops restricting her diet, but due to the physiological and psychological changes that have taken place from the initial rapid weight loss this quickly results in weight regain. Sharon is now at a higher weight than when she first went to the doctor for her ankle. Weight gain leaves Sharon feeling more helpless and frustrated, leading to personal and social shame. Sharon finds herself emotionally eating for the first time in her life. Sharon’s stress continues to impact her physical and mental body in a vicious cycle of dieting and over eating. She is in a constant fight between body and mind as she struggles to meet an unrealistic weight ideal. Sharon was a healthy, happy fat women, now she is an unhealthy, unhappy fat women.
According to Tatiana, et al. (2012), “The prevalence of weight/height discrimination increased from 7% in 1995–1996 to 12% in 2004–2006, affecting all population groups but the elderly.” This research disassociated this increase to any increases in obesity rates over the same time frame.
It is alarming to think that so many people feel it is okay, and even expected, to make others feel humiliated for being fat.
How do we switch the paradigm that has become increasingly engrained in us that fat is bad?
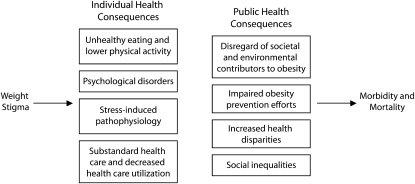
Figure 1: Individual and public health consequences of weight stigma (Rebecca M. et al.)
Our genetic make-up predisposes us to our physical selves, such that we cannot change. It is our environment(s) and experiences within them that influence our choices, habits, and emotional reactions. If you were born into a large body, which you cannot change, then criticized for it and told to change or else…! you are destined for hardship.
However, if you were born into a large body, which you cannot change, and given tools, resources, and support to be the best version of you, no matter what your weight, you could do it.
I am not saying that if you adopt healthier habits that you will, won’t or shouldn’t lose weight, I am saying that should not be the goal. If you feel healthy, if you feel happy, why does it matter what your weight is? If you do not feel healthy, if you do not feel happy, it still doesn’t matter what your weight is; it matters what efforts you put in to adapt a lifestyle that supports a healthy and happy you.

What is a Healthy Body and Mind (to you)?
Lifestyle habits, including those that affect our mental as well as physical health, are ultimately what forms our overall wellbeing NOT what fad diet we are on, or how much weight we have lost, or gained, over the last month.
Once we can all shake the notion that weight is the end all of health and happiness we can move on to truly listening to our wants and needs as unique individuals.
Regularly checking in with yourself to determine what healthy means to you is an important piece of this. Be realistic with yourself about how you feel, what you want. Ask yourself often: are there areas to improve that could enhance my overall wellbeing to ensure I am still living the best life I can?
Conclusion
There is no one thing to blame for how wide and deep weight bias has spread. As stated in the article Weight Bias: A Call to Action, “…the complexity of obesity lies beyond the individual” (Angela Alberga et al.) No matter how we got here, getting away from weight stigmatization and discrimination has to be population-wide, from health care workers to co-worker to friends and family alike. And that includes you.
Focus on health, focus on happiness; work towards want you want out of life and weight will be a concern of the past.

Recommendations to wait on weight, for anyone, of any size:
- Don’t weight yourself. Ask to not be weighed at the doctors off, or if they have to because of the reason for your visit, ask not to see or be told your weight.
- Think before you speak. Even a positive comment made with good intention can have negative consequences. Such as praising a coworker for losing weight sends the message that they were doing something wrong before becoming thinner, or that being thinner is somehow better than being larger. This only strengthens the stigma. Any general comment made about body size may fall on sensitive ears and add to weight bias.
- Check your bias. Do you think about fat people differently or treat them differently? Why? How can you use this bias awareness to improve your actions to mitigate weight stigma? To get started, take Harvard’s Implicit Association Test on weight: https://implicit.harvard.edu/implicit/Study?tid=-1
- Speak up! If you feel you are being stigmatized, or treated unfairly because of your body weight. Or, if you see others acting in this way. Most people do not speak or act in offensive ways on purpose and truly want to act appropriately; their weight bias is likely implicit until someone brings it to their attention. Kindly explaining how their action or comment made you, or may make others, feel is a step in the right direction.

References and Resources:
Angela S. Alberga, Shelly Russell-Mayhew, Kristin M. von Ranson and Lindsay McLaren. Weight bias: a call to action. Journal of Eating Disorders (2016) 4:34, DOI 10.1186/s40337-016-0112-4. Online at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5100338/pdf/40337_2016_Article_112.pdf
Rebecca M. Puhl, PhD, and Chelsea A. Heuer, MPH. Obesity Stigma: Important Considerations for Public Health. American Journal of Public Health June 2010, 100 (6). Online at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2866597/pdf/1019.pdf
Maya Vadiveloo, PhD RD & Josiemer Mattei PhD MPH. Perceived Weight Discrimination and 10 year Risk of Allostatic Load among US Adults. Ann. Behav. Med. (2017) 51:94-104. DOI: 10.1007/s12160-016-9831-7.
A. Janet Tomiyama. Weight stigma is stressful. A review of evidence for the Cyclic
Obesity/Weight-Based Stigma model. Appetite 82 (2014) 8–15. Online at: http://www.dishlab.org/pubs/Tomiyama%20COBWEBS.pdf
Stella Medvedyuk, Ahmednur Ali & Dennis Raphael (2017). Ideology, obesity and the social determinants of health: A critical analysis of the obesity and health relationship. Critical Public Health, DOI: 10.1080/09581596.2017.1356910
Tatiana Andreyeva, Rebecca M. Puhl & Kelly D. Brownell. Changes in Perceived Weight Discrimination Among Americans, 1995–1996 Through 2004–2006. Obesity (2008) 16, 1129–1134. https://doi.org/10.1038/oby.2008.35
UCONN Rudd Center for Food Policy and Obesity: Weight Bias & Stigma. http://uconnruddcenter.org/weight-bias-stigma
Jes Baker, The Militant Baker: http://www.themilitantbaker.com/p/about.html

